Bronchiectasis (brong-ke-EK-ta-sis)
is a condition in which damage to the airways causes them to widen and become flabby and scarred. The airways are tubes that carry air in and out of your lungs.
Bronchiectasis usually is the result of an infection or other condition that injures the walls of your airways or prevents the airways from clearing mucus. Mucus is a slimy substance that the airways produce to help remove inhaled dust, bacteria, and other small particles.
In bronchiectasis, your airways slowly lose their ability to clear out mucus. When mucus can’t be cleared, it builds up and creates an environment in which bacteria can grow. This leads to repeated, serious lung infections.
Each infection causes more damage to your airways. Over time, the airways lose their ability to move air in and out. This can prevent enough oxygen from reaching your vital organs.
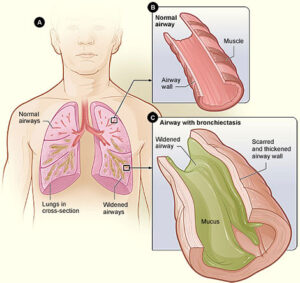
Figure A shows a cross-section of the lungs with normal airways and with widened airways. Figure B shows a cross-section of a normal airway. Figure C shows a cross-section of an airway with bronchiectasis.
Bronchiectasis can lead to serious health problems, such as respiratory failure, atelectasis (at-eh-LEK-tah-sis), and heart failure.
Overview
Bronchiectasis can affect just one section of one of your lungs or many sections of both lungs.
The initial lung damage that leads to bronchiectasis often begins in childhood. However, symptoms may not occur until months or even years after you start having repeated lung infections.
In the United States, common childhood infections-such as whooping cough and measles-used to cause many cases of bronchiectasis. However, these causes are now less common because of vaccines and antibiotics.
Now bronchiectasis usually is due to a medical condition that injures the airway walls or prevents the airways from clearing mucus. Examples of such conditions include cystic fibrosis and primary ciliary (SIL-e-ar-e) dyskinesia (dis-kih-NE-ze-ah), or PCD.
Bronchiectasis that affects only one part of the lung may be caused by a blockage rather than a medical condition.
Bronchiectasis can be congenital (kon-JEN-ih-tal) or acquired. Congenital bronchiectasis affects infants and children. It’s the result of a problem with how the lungs form in a fetus.
Acquired bronchiectasis occurs as a result of another condition or factor. This type of bronchiectasis can affect adults and older children. Acquired bronchiectasis is more common than the congenital type.
Outlook
Currently, bronchiectasis has no cure. However, with proper care, most people who have it can enjoy a good quality of life.
Early diagnosis and treatment of bronchiectasis are important. The sooner your doctor starts treating bronchiectasis and any underlying conditions, the better your chances of preventing further lung damage.
Damage to the walls of the airways usually is the cause of bronchiectasis. A lung infection may cause this damage. Examples of lung infections that can lead to bronchiectasis include:
- Severe pneumonia (nu-MO-ne-ah)
- Whooping cough or measles (uncommon in the United States due to vaccination)
- Tuberculosis
- Fungal infections
Conditions that damage the airways and raise the risk of lung infections also can lead to bronchiectasis. Examples of such conditions include:
- Cystic fibrosis. This disease leads to almost half of the cases of bronchiectasis in the United States.
- Immunodeficiency disorders, such as common variable immunodeficiency and, less often, HIV and AIDS.
- Allergic bronchopulmonary aspergillosis (AS-per-ji-LO-sis). This is an allergic reaction to a fungus called aspergillus. The reaction causes swelling in the airways.
- Disorders that affect cilia (SIL-e-ah) function, such as primary ciliary dyskinesia. Cilia are small, hair-like structures that line your airways. They help clear mucus (a slimy substance) out of your airways.
- Chronic (ongoing) pulmonary aspiration (as-pih-RA-shun). This is a condition in which you inhale food, liquids, saliva, or vomited stomach contents into your lungs. Aspiration can inflame the airways, which can lead to bronchiectasis.
- Connective tissue diseases, such as rheumatoid arthritis, Sjogren’s syndrome, and Crohn ‘s disease.
Other conditions, such as an airway blockage, also can lead to bronchiectasis. Many things can cause a blockage, such as a growth or a noncancerous tumor. An inhaled object, such as a piece of a toy or a peanut that you inhaled as a child, also can cause an airway blockage.
A problem with how the lungs form in a fetus may cause congenital bronchiectasis. This condition affects infants and children.
People who have conditions that damage the lungs or increase the risk of lung infections are at risk for bronchiectasis. Such conditions include:
- Cystic fibrosis. This disease leads to almost half of the cases of bronchiectasis in the United States.
- Immunodeficiency disorders, such as common variable immunodeficiency and, less often, HIV and AIDS.
- Allergic bronchopulmonary aspergillosis. This is an allergic reaction to a fungus called aspergillus. The reaction causes swelling in the airways.
- Disorders that affect cilia function, such as primary ciliary dyskinesia. Cilia are small, hair-like structures that line your airways. They help clear mucus (a slimy substance) out of your airways.
Bronchiectasis can develop at any age. Overall, two-thirds of people who have the condition are women. However, in children, the condition is more common in boys than in girls.
The initial airway damage that leads to bronchiectasis often begins in childhood. However, signs and symptoms may not appear until months or even years after you start having repeated lung infections.
The most common signs and symptoms of bronchiectasis are:
- A daily cough that occurs over months or years.
- Daily production of large amounts of sputum (spit). Sputum, which you cough up and spit out, may contain mucus (a slimy substance), trapped particles, and pus.
- Shortness of breath and wheezing (a whistling sound when you breathe).
- Chest pain.
- Clubbing (the flesh under your fingernails and toenails gets thicker)
If your doctor listens to your lungs with a stethoscope, he or she may hear abnormal lung sounds.
Over time, you may have more serious symptoms. You may cough up blood or bloody mucus and feel very tired. Children may lose weight or not grow at a normal rate.
Complications of Bronchiectasis
Severe bronchiectasis can lead to other serious health conditions, such as respiratory failure and atelectasis.
Respiratory failure is a condition in which not enough oxygen passes from your lungs into your blood. The condition also can occur if your lungs can’t properly remove carbon dioxide (a waste gas) from your blood.
Respiratory failure can cause shortness of breath, rapid breathing, and air hunger (feeling like you can’t breathe in enough air). In severe cases, signs and symptoms may include a bluish color on your skin, lips, and fingernails; confusion; and sleepiness.
Atelectasis is a condition in which one or more areas of your lungs collapse or don’t inflate properly. As a result, you may feel short of breath. Your heart rate and breathing rate may increase, and your skin and lips may turn blue.
If bronchiectasis is so advanced that it affects all parts of your airways, it may cause heart failure. Heart failure is a condition in which the heart can’t pump enough blood to meet the body’s needs.
The most common signs and symptoms of heart failure are shortness of breath or trouble breathing, tiredness, and swelling in the ankles, feet, legs, abdomen, and veins in the neck.
Your doctor may suspect bronchiectasis if you have a daily cough that produces large amounts of sputum (spit).
To find out whether you have bronchiectasis, your doctor may recommend tests to:
- Identify any underlying causes that require treatment
- Rule out other causes of your symptoms
- Find out how much your airways are damaged
Diagnostic Tests and Procedures
Chest CT Scan
A chest computed tomography (to-MOG-ra-fee) scan, or chest CT scan, is the most common test for diagnosing bronchiectasis.
This painless test creates precise pictures of your airways and other structures in your chest. A chest CT scan can show the extent and location of lung damage. This test gives more detailed pictures than a standard chest x ray.
Chest X Ray
This painless test creates pictures of the structures in your chest, such as your heart and lungs. A chest x ray can show areas of abnormal lung and thickened, irregular airway walls.
Other Tests
- Blood tests. These tests can show whether you have an underlying condition that can lead to bronchiectasis. Blood tests also can show whether you have an infection or low levels of certain infection-fighting blood cells.
- A sputum culture. Lab tests can show whether a sample of your sputum contains bacteria (such as the bacteria that cause tuberculosis) or fungi.
- Lung function tests. These tests measure how much air you can breathe in and out, how fast you can breathe air out, and how well your lungs deliver oxygen to your blood. Lung function tests help show how much lung damage you have.
- A sweat test or other tests for cystic fibrosis.
Bronchoscopy
If your bronchiectasis doesn’t respond to treatment, your doctor may recommend bronchoscopy (bron-KOS-ko-pee). Doctors use this procedure to look inside the airways.
During bronchoscopy, a flexible tube with a light on the end is inserted through your nose or mouth into your airways. The tube is called a bronchoscope. It provides a video image of your airways. You’ll be given medicine to numb your upper airway and help you relax during the procedure.
Bronchoscopy can show whether you have a blockage in your airways. The procedure also can show the source of any bleeding in your airways.
Bronchiectasis often is treated with medicines, hydration, and chest physical therapy (CPT). Your doctor may recommend surgery if the bronchiectasis is isolated to a section of lung or you have a lot of bleeding.
If the bronchiectasis is widespread and causing respiratory failure, your doctor may recommend oxygen therapy.
The goals of treatment are to:
- Treat any underlying conditions and lung infections.
- Remove mucus (a slimy substance) from your lungs. Maintaining good hydration helps with mucus removal.
- Prevent complications.
Early diagnosis and treatment of the underlying cause of bronchiectasis may help prevent further lung damage.
In addition, any disease associated with the bronchiectasis, such as cystic fibrosis or immunodeficiency, also should be treated.
Medicines
Your doctor may prescribe antibiotics, bronchodilators, expectorants, or mucus-thinning medicines to treat bronchiectasis.
Antibiotics
Antibiotics are the main treatment for the repeated lung infections that bronchiectasis causes. Oral antibiotics often are used to treat these infections.
For hard-to-treat infections, your doctor may prescribe intravenous (IV) antibiotics. These medicines are given through an IV line inserted into your arm. Your doctor may help you arrange for a home care provider to give you IV antibiotics at home.
Expectorants and Mucus-Thinning Medicines
Your doctor may prescribe expectorants and mucus thinners to help you cough up mucus.
Expectorants help loosen the mucus in your lungs. They often are combined with decongestants, which may provide extra relief. Mucus thinners, such as acetylcysteine, loosen the mucus to make it easier to cough up.
For some of these treatments, little information is available to show how well they work.
Hydration
Drinking plenty of fluid, especially water, helps prevent airway mucus from becoming thick and sticky. Good hydration helps keep airway mucus moist and slippery, which makes it easier to cough up.
Chest Physical Therapy
CPT also is called physiotherapy (FIZ-e-o-THER-ah-pe) or chest clapping or percussion. This technique is generally performed by a respiratory therapist but can be done by a trained member of the family. It involves the therapist pounding your chest and back over and over with his or her hands or a device. Doing this helps loosen the mucus from your lungs so you can cough it up.
You can sit with your head tilted down or lie on your stomach with your head down while you do CPT. Gravity and force help drain the mucus from your lungs.
Some people find CPT hard or uncomfortable to do. Several devices can help with CPT, such as:
- An electric chest clapper, known as a mechanical percussor.
- An inflatable therapy vest that uses high-frequency air waves to force mucus toward your upper airways so you can cough it up.
- A small handheld device that you breathe out through. It causes vibrations that dislodge the mucus.
- A mask that creates vibrations to help break loose mucus from your airway walls.
Some of these methods and devices are popular with patients and doctors, but little information is available on how well they actually work. Choice usually is based on convenience and cost.
Several breathing techniques also are used to help move mucus to the upper airway so it can be coughed up. These techniques include forced expiration technique (FET) and active cycle breathing (ACB).
FET involves forcing out a couple of breaths and then doing relaxed breathing. ACB is FET that involves deep breathing exercises.
Other Treatments
Depending on your condition, your doctor also may recommend bronchodilators, inhaled corticosteroids, oxygen therapy, or surgery.
Bronchodilators
Bronchodilators relax the muscles around your airways. This helps open your airways and makes breathing easier. Most bronchodilators are inhaled medicines. You will use an inhaler or a nebulizer to breathe in a fine mist of medicine.
Inhaled bronchodilators work quickly because the medicine goes straight to your lungs. Your doctor may recommend that you use a bronchodilator right before you do CPT.
Inhaled Corticosteroids
If you also have wheezing or asthma with your bronchiectasis, your doctor may prescribe inhaled corticosteroids (used to treat inflammation in the airways).
Oxygen Therapy
Oxygen therapy can help raise low blood oxygen levels. For this treatment, you’ll receive oxygen through nasal prongs or a mask. Oxygen therapy can be done at home, in a hospital, or in another health facility.
Surgery
Your doctor may recommend surgery if no other treatments have helped and only one part of your airway is affected. If you have major bleeding in your airway, your doctor may recommend surgery to remove part of your airway or a procedure to control the bleeding.
In very rare instances of severe bronchiectasis, your doctor may recommend that you receive a lung transplant replacing your diseased lungs with a healthy set of lungs.
To prevent bronchiectasis, it’s important to prevent the lung infections and lung damage that can cause it.
Childhood vaccines for measles and whooping cough prevent infections related to these illnesses. These vaccines also reduce complications from these infections, such as bronchiectasis.
Avoiding toxic fumes, gases, smoke, and other harmful substances also can help protect your lungs.
Proper treatment of lung infections in children also may help preserve lung function and prevent lung damage that can lead to bronchiectasis.
Stay alert to keep children (and adults) from inhaling small objects (such as pieces of toys and food that might stick in a small airway). If you think you, your child, or someone else has inhaled a small object, seek prompt medical care.
In some cases, treating the underlying cause of bronchiectasis can slow or prevent its progression.
Early diagnosis and treatment of bronchiectasis can prevent further damage to your lungs. People who have bronchiectasis should have ongoing care and try to follow a healthy lifestyle.
Ongoing Care
If you have bronchiectasis, work closely with your doctor to learn how to improve your quality of life. This involves learning as much as you can about bronchiectasis and any underlying conditions that you have.
Take steps to avoid lung infections. Ask your doctor about getting flu and pneumonia vaccines. Wash your hands often to lower your risk of getting viruses and bacterial infections.
Healthy Lifestyle
Following a healthy lifestyle is important for overall health and well-being. For example, if you smoke, try to quit. Smoking harms nearly every organ in your body, including your lungs.
Talk with your doctor about programs and products that can help you quit smoking. Also, try to avoid secondhand smoke.
If you have trouble quitting smoking on your own, consider joining a support group. Many hospitals, workplaces, and community groups offer classes to help people quit smoking.
You also can protect your airways by avoiding toxic fumes, gases, and other harmful substances.
A healthy lifestyle also involves following a healthy diet. A healthy diet includes a variety of vegetables and fruits. It also includes whole grains, fat-free or low-fat dairy products, and protein foods, such as lean meats, poultry without skin, seafood, processed soy products, nuts, seeds, beans, and peas.
A healthy diet is low in sodium (salt), added sugars, solid fats, and refined grains. Solid fats are saturated fat and trans fatty acids. Refined grains come from processing whole grains, which results in a loss of nutrients (such as dietary fiber).
Staying hydrated also is important. Drinking plenty of fluids, especially water, helps prevent airway mucus from becoming thick and sticky.
Try to be as physically active as you can. Physical activity, such as walking and swimming, can help loosen mucus. Ask your doctor what types and amounts of activity are safe for you.
Emotional Support
People who have chronic lung diseases are more prone to depression, anxiety, and other emotional problems. Talk about how you feel with your health care team. Talking to a professional counselor also can help. If you’re very depressed, your doctor may recommend medicines or other treatments that can improve your quality of life.
Joining a patient support group may help you adjust to living with bronchiectasis. You can see how other people who have the same symptoms have coped with them. Talk with your doctor about local support groups or check with an area medical center.
Support from family and friends also can help relieve stress and anxiety. Let your loved ones know how you feel and what they can do to help you.