Asthma (AZ-ma) is a chronic (long-term) lung disease that inflames and narrows the airways. Asthma causes recurring periods of wheezing (a whistling sound when you breathe), chest tightness, shortness of breath, and coughing. The coughing often occurs at night or early in the morning.
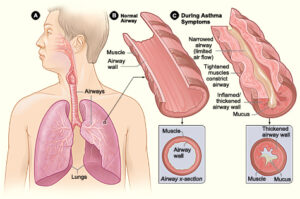
Figure A shows the location of the lungs and airways in the body. Figure B shows a cross-section of a normal airway. Figure C shows a cross-section of an airway during asthma symptoms.
Asthma affects people of all ages, but it most often starts during childhood. In the United States, more than 25 million people are known to have asthma. About 7 million of these people are children.
Overview
To understand asthma, it helps to know how the airways work. The airways are tubes that carry air into and out of your lungs. People who have asthma have inflamed airways. The inflammation makes the airways swollen and very sensitive. The airways tend to react strongly to certain inhaled substances.
When the airways react, the muscles around them tighten. This narrows the airways, causing less air to flow into the lungs. The swelling also can worsen, making the airways even narrower. Cells in the airways might make more mucus than usual. Mucus is a sticky, thick liquid that can further narrow the airways.
This chain reaction can result in asthma symptoms. Symptoms can happen each time the airways are inflamed.
Sometimes asthma symptoms are mild and go away on their own or after minimal treatment with asthma medicine. Other times, symptoms continue to get worse.
When symptoms get more intense and/or more symptoms occur, you’re having an asthma attack. Asthma attacks also are called flareups or exacerbations (eg-zas-er-BA-shuns).
Treating symptoms when you first notice them is important. This will help prevent the symptoms from worsening and causing a severe asthma attack. Severe asthma attacks may require emergency care, and they can be fatal.
Outlook
Asthma has no cure. Even when you feel fine, you still have the disease and it can flare up at any time.
However, with today’s knowledge and treatments, most people who have asthma are able to manage the disease. They have few, if any, symptoms. They can live normal, active lives and sleep through the night without interruption from asthma.
If you have asthma, you can take an active role in managing the disease. For successful, thorough, and ongoing treatment, build strong partnerships with your doctor and other health care providers.
The exact cause of asthma isn’t known. Researchers think some genetic and environmental factors interact to cause asthma, most often early in life. These factors include:
- An inherited tendency to develop allergies, called atopy (AT-o-pe)
- Parents who have asthma
- Certain respiratory infections during childhood
- Contact with some airborne allergens or exposure to some viral infections in infancy or in early childhood when the immune system is developing
If asthma or atopy runs in your family, exposure to irritants (for example, tobacco smoke) may make your airways more reactive to substances in the air.
Some factors may be more likely to cause asthma in some people than in others. Researchers continue to explore what causes asthma.
The “Hygiene Hypothesis”
One theory researchers have for what causes asthma is the “hygiene hypothesis.” They believe that our Western lifestyle—with its emphasis on hygiene and sanitation—has resulted in changes in our living conditions and an overall decline in infections in early childhood.
Many young children no longer have the same types of environmental exposures and infections as children did in the past. This affects the way that young children’s immune systems develop during very early childhood, and it may increase their risk for atopy and asthma. This is especially true for children who have close family members with one or both of these conditions.
Asthma affects people of all ages, but it most often starts during childhood. In the United States, more than 22 million people are known to have asthma. Nearly 6 million of these people are children.
Young children who often wheeze and have respiratory infections-as well as certain other risk factors-are at highest risk of developing asthma that continues beyond 6 years of age. The other risk factors include having allergies, eczema (an allergic skin condition), or parents who have asthma.
Among children, more boys have asthma than girls. But among adults, more women have the disease than men. It’s not clear whether or how sex and sex hormones play a role in causing asthma.
Most, but not all, people who have asthma have allergies.
Some people develop asthma because of contact with certain chemical irritants or industrial dusts in the workplace. This type of asthma is called occupational asthma.
Common signs and symptoms of asthma include:
- Coughing. Coughing from asthma often is worse at night or early in the morning, making it hard to sleep.
- Wheezing. Wheezing is a whistling or squeaky sound that occurs when you breathe.
- Chest tightness. This may feel like something is squeezing or sitting on your chest.
- Shortness of breath. Some people who have asthma say they can’t catch their breath or they feel out of breath. You may feel like you can’t get air out of your lungs.
Not all people who have asthma have these symptoms. Likewise, having these symptoms doesn’t always mean that you have asthma. The best way to diagnose asthma for certain is to use a lung function test, a medical history (including type and frequency of symptoms), and a physical exam.
The types of asthma symptoms you have, how often they occur, and how severe they are may vary over time. Sometimes your symptoms may just annoy you. Other times, they may be troublesome enough to limit your daily routine.
Severe symptoms can be fatal. It’s important to treat symptoms when you first notice them so they don’t become severe.
With proper treatment, most people who have asthma can expect to have few, if any, symptoms either during the day or at night.
What Causes Asthma Symptoms To Occur?
Many things can trigger or worsen asthma symptoms. Your doctor will help you find out which things (sometimes called triggers) may cause your asthma to flare up if you come in contact with them. Triggers may include:
- Allergens from dust, animal fur, cockroaches, mold, and pollens from trees, grasses, and flowers
- Irritants such as cigarette smoke, air pollution, chemicals or dust in the workplace, compounds in home decore products, and sprays (such as hairspray)
- Medicines such as aspirin or other nonsteroidal anti-inflammatory drugs and nonselective beta-blockers
- Sulfites in foods and drinks
- Viral upper respiratory infections, such as colds
- Physical activity, including exercise
Other health conditions can make asthma harder to manage. Examples of these conditions include a runny nose, sinus infections, reflux disease, psychological stress, and sleep apnea. These conditions need treatment as part of an overall asthma care plan.
Asthma is different for each person. Some of the triggers listed above may not affect you. Other triggers that do affect you may not be on the list. Talk with your doctor about the things that seem to make your asthma worse.
Your primary care doctor will diagnose asthma based on your medical and family histories, a physical exam, and test results.
Your doctor also will figure out the severity of your asthma-that is, whether it’s intermittent, mild, moderate, or severe. The level of severity will determine what treatment you’ll start on.
You may need to see an asthma specialist if:
- You need special tests to help diagnose asthma
- You’ve had a life-threatening asthma attack
- You need more than one kind of medicine or higher doses of medicine to control your asthma, or if you have overall problems getting your asthma well controlled
- You’re thinking about getting allergy treatments
Medical and Family Histories
Your doctor may ask about your family history of asthma and allergies. He or she also may ask whether you have asthma symptoms and when and how often they occur.
Let your doctor know whether your symptoms seem to happen only during certain times of the year or in certain places, or if they get worse at night.
Your doctor also may want to know what factors seem to trigger your symptoms or worsen them.
Your doctor may ask you about related health conditions that can interfere with asthma management. These conditions include a runny nose, sinus infections, reflux disease, psychological stress, and sleep apnea.
Physical Exam
Your doctor will listen to your breathing and look for signs of asthma or allergies. These signs include wheezing, a runny nose or swollen nasal passages, and allergic skin conditions (such as eczema).
Keep in mind that you can still have asthma even if you don’t have these signs on the day that your doctor examines you.
Diagnostic Tests
Lung Function Test
Your doctor will use a test called spirometry (spi-ROM-eh-tre) to check how your lungs are working. This test measures how much air you can breathe in and out. It also measures how fast you can blow air out.
Your doctor also may give you medicine and then test you again to see whether the results have improved.
If the starting results are lower than normal and improve with the medicine, and if your medical history shows a pattern of asthma symptoms, your diagnosis will likely be asthma.
Other Tests
Your doctor may recommend other tests if he or she needs more information to make a diagnosis. Other tests may include:
- Allergy testing to find out which allergens affect you, if any.
- A test to measure how sensitive your airways are. This is called a bronchoprovocation (brong-KO-prav-eh-KA-shun) test. Using spirometry, this test repeatedly measures your lung function during physical activity or after you receive increasing doses of cold air or a special chemical to breathe in.
- A test to show whether you have another condition with the same symptoms as asthma, such as reflux disease, vocal cord dysfunction, or sleep apnea.
- A chest x ray or an EKG (electrocardiogram). These tests will help find out whether a foreign object or other disease may be causing your symptoms.
Diagnosing Asthma in Young Children
Most children who have asthma develop their first symptoms before 5 years of age. However, asthma in young children (aged 0 to 5 years) can be hard to diagnose.
Sometimes it’s hard to tell whether a child has asthma or another childhood condition. This is because the symptoms of asthma also occur with other conditions.
Also, many young children who wheeze when they get colds or respiratory infections don’t go on to have asthma after they’re 6 years old.
A child may wheeze because he or she has small airways that become even narrower during colds or respiratory infections. The airways grow as the child grows older, so wheezing no longer occurs when the child gets colds.
A young child who has frequent wheezing with colds or respiratory infections is more likely to have asthma if:
- One or both parents have asthma
- The child has signs of allergies, including the allergic skin condition eczema
- The child has allergic reactions to pollens or other airborne allergens
- The child wheezes even when he or she doesn’t have a cold or other infection
The most certain way to diagnose asthma is with a lung function test, a medical history, and a physical exam. However, it’s hard to do lung function tests in children younger than 5 years. Thus, doctors must rely on children’s medical histories, signs and symptoms, and physical exams to make a diagnosis.
Doctors also may use a 4-6 week trial of asthma medicines to see how well a child responds.
Asthma is a long-term disease that has no cure. The goal of asthma treatment is to control the disease. Good asthma control will:
- Prevent chronic and troublesome symptoms, such as coughing and shortness of breath
- Reduce your need for quick-relief medicines (see below)
- Help you maintain good lung function
- Let you maintain your normal activity level and sleep through the night
- Prevent asthma attacks that could result in an emergency room visit or hospital stay
To control asthma, partner with your doctor to manage your asthma or your child’s asthma. Children aged 10 or older-and younger children who are able-should take an active role in their asthma care.
Taking an active role to control your asthma involves:
- Working with your doctor to treat other conditions that can interfere with asthma management.
- Avoiding things that worsen your asthma (asthma triggers). However, one trigger you should not avoid is physical activity. Physical activity is an important part of a healthy lifestyle. Talk with your doctor about medicines that can help you stay active.
- Working with your doctor and other health care providers to create and follow an asthma action plan.
An asthma action plan gives guidance on taking your medicines properly, avoiding asthma triggers (except physical activity), tracking your level of asthma control, responding to worsening symptoms, and seeking emergency care when needed.
Asthma is treated with two types of medicines: long-term control and quick-relief medicines. Long-term control medicines help reduce airway inflammation and prevent asthma symptoms. Quick-relief, or “rescue,” medicines relieve asthma symptoms that may flare up.
Your initial treatment will depend on the severity of your asthma. Followup asthma treatment will depend on how well your asthma action plan is controlling your symptoms and preventing asthma attacks.
Your level of asthma control can vary over time and with changes in your home, school, or work environments. These changes can alter how often you’re exposed to the factors that can worsen your asthma.
Your doctor may need to increase your medicine if your asthma doesn’t stay under control. On the other hand, if your asthma is well controlled for several months, your doctor may decrease your medicine. These adjustments to your medicine will help you maintain the best control possible with the least amount of medicine necessary.
Asthma treatment for certain groups of people-such as children, pregnant women, or those for whom exercise brings on asthma symptoms-will be adjusted to meet their special needs.
Follow an Asthma Action Plan
You can work with your doctor to create a personal asthma action plan. The plan will describe your daily treatments, such as which medicines to take and when to take them. The plan also will explain when to call your doctor or go to the emergency room.
If your child has asthma, all of the people who care for him or her should know about the child’s asthma action plan. This includes babysitters and workers at daycare centers, schools, and camps. These caretakers can help your child follow his or her action plan.
Avoid Things That Can Worsen Your Asthma
Many common things (called asthma triggers) can set off or worsen your asthma symptoms. Once you know what these things are, you can take steps to control many of them.
For example, exposure to pollens or air pollution might make your asthma worse. If so, try to limit time outdoors when the levels of these substances in the outdoor air are high. If animal fur triggers your asthma symptoms, keep pets with fur out of your home or bedroom.
One possible asthma trigger you shouldn’t avoid is physical activity. Physical activity is an important part of a healthy lifestyle. Talk with your doctor about medicines that can help you stay active.
If your asthma symptoms are clearly related to allergens, and you can’t avoid exposure to those allergens, your doctor may advise you to get allergy shots.
You may need to see a specialist if you’re thinking about getting allergy shots. These shots can lessen or prevent your asthma symptoms, but they can’t cure your asthma.
Several health conditions can make asthma harder to manage. These conditions include runny nose, sinus infections, reflux disease, psychological stress, and sleep apnea. Your doctor will treat these conditions as well.
Medicines
Your doctor will consider many things when deciding which asthma medicines are best for you. He or she will check to see how well a medicine works for you. Then, he or she will adjust the dose or medicine as needed.
Asthma medicines can be taken in pill form, but most are taken using a device called an inhaler. An inhaler allows the medicine to go directly to your lungs.
Not all inhalers are used the same way. Ask your doctor or another health care provider to show you the right way to use your inhaler. Review the way you use your inhaler at every medical visit.
Long-Term Control Medicines
Most people who have asthma need to take long-term control medicines daily to help prevent symptoms. The most effective long-term medicines reduce airway inflammation, which helps prevent symptoms from starting. These medicines don’t give you quick relief from symptoms.
Inhaled corticosteroids.
Inhaled corticosteroids are the preferred medicine for long-term control of asthma. They’re the most effective option for long-term relief of the inflammation and swelling that makes your airways sensitive to certain inhaled substances.
Reducing inflammation helps prevent the chain reaction that causes asthma symptoms. Most people who take these medicines daily find they greatly reduce the severity of symptoms and how often they occur.
Inhaled corticosteroids generally are safe when taken as prescribed. These medicines are different from the illegal anabolic steroids taken by some athletes. Inhaled corticosteroids aren’t habit-forming, even if you take them every day for many years.
Like many other medicines, though, inhaled corticosteroids can have side effects. Most doctors agree that the benefits of taking inhaled corticosteroids and preventing asthma attacks far outweigh the risk of side effects.
One common side effect from inhaled corticosteroids is a mouth infection called thrush. You might be able to use a spacer or holding chamber on your inhaler to avoid thrush. These devices attach to your inhaler. They help prevent the medicine from landing in your mouth or on the back of your throat.
Check with your doctor to see whether a spacer or holding chamber should be used with the inhaler you have. Also, work with your health care team if you have any questions about how to use a spacer or holding chamber. Rinsing your mouth out with water after taking inhaled corticosteroids also can lower your risk for thrush.
If you have severe asthma, you may have to take corticosteroid pills or liquid for short periods to get your asthma under control.
If taken for long periods, these medicines raise your risk for cataracts and osteoporosis (OS-te-o-po-RO-sis). A cataract is the clouding of the lens in your eye. Osteoporosis is a disorder that makes your bones weak and more likely to break.
Your doctor may have you add another long-term asthma control medicine so he or she can lower your dose of corticosteroids. Or, your doctor may suggest you take calcium and vitamin D pills to protect your bones.
Other long-term control medicines.
Other long-term control medicines include:
- Cromolyn. This medicine is taken using a device called a nebulizer. As you breathe in, the nebulizer sends a fine mist of medicine to your lungs. Cromolyn helps prevent airway inflammation.
- Omalizumab (anti-IgE). This medicine is given as a shot (injection) one or two times a month. It helps prevent your body from reacting to asthma triggers, such as pollen and dust mites. Anti-IgE might be used if other asthma medicines have not worked well.
A rare, but possibly life-threatening allergic reaction called anaphylaxis might occur when the Omalizumab injection is given. If you take this medication, work with your doctor to make sure you understand the signs and symptoms of anaphylaxis and what actions you should take.
- Inhaled long-acting beta2-agonists. These medicines open the airways. They might be added to inhaled corticosteroids to improve asthma control. Inhaled long-acting beta2-agonists should never be used on their own for long-term asthma control. They must used with inhaled corticosteroids.
- Leukotriene modifiers. These medicines are taken by mouth. They help block the chain reaction that increases inflammation in your airways.
- Theophylline. This medicine is taken by mouth. Theophylline helps open the airways.
If your doctor prescribes a long-term control medicine, take it every day to control your asthma. Your asthma symptoms will likely return or get worse if you stop taking your medicine.
Long-term control medicines can have side effects. Talk with your doctor about these side effects and ways to reduce or avoid them.
With some medicines, like theophylline, your doctor will check the level of medicine in your blood. This helps ensure that you’re getting enough medicine to relieve your asthma symptoms, but not so much that it causes dangerous side effects.
Quick-Relief Medicines
All people who have asthma need quick-relief medicines to help relieve asthma symptoms that may flare up. Inhaled short-acting beta2-agonists are the first choice for quick relief.
These medicines act quickly to relax tight muscles around your airways when you’re having a flareup. This allows the airways to open up so air can flow through them.
You should take your quick-relief medicine when you first notice asthma symptoms. If you use this medicine more than 2 days a week, talk with your doctor about your asthma control. You may need to make changes to your asthma action plan.
Carry your quick-relief inhaler with you at all times in case you need it. If your child has asthma, make sure that anyone caring for him or her has the child’s quick-relief medicines, including staff at the child’s school. They should understand when and how to use these medicines and when to seek medical care for your child.
You shouldn’t use quick-relief medicines in place of prescribed long-term control medicines. Quick-relief medicines don’t reduce inflammation.
Track Your Asthma
To track your asthma, keep records of your symptoms, check your peak flow number using a peak flow meter, and get regular asthma checkups.
Record Your Symptoms
You can record your asthma symptoms in a diary to see how well your treatments are controlling your asthma.
Asthma is well controlled if:
- You have symptoms no more than 2 days a week, and these symptoms don’t wake you from sleep more than 1 or 2 nights a month.
- You can do all your normal activities.
- You take quick-relief medicines no more than 2 days a week.
- You have no more than one asthma attack a year that requires you to take corticosteroids by mouth.
- Your peak flow doesn’t drop below 80 percent of your personal best number.
If your asthma isn’t well controlled, contact your doctor. He or she may need to change your asthma action plan.
Use a Peak Flow Meter
This small, hand-held device shows how well air moves out of your lungs. You blow into the device and it gives you a score, or peak flow number. Your score shows how well your lungs are working at the time of the test.
Your doctor will tell you how and when to use your peak flow meter. He or she also will teach you how to take your medicines based on your score.
Your doctor and other health care providers may ask you to use your peak flow meter each morning and keep a record of your results. You may find it very useful to record peak flow scores for a couple of weeks before each medical visit and take the results with you.
When you’re first diagnosed with asthma, it’s important to find your “personal best” peak flow number. To do this, you record your score each day for a 2- to 3-week period when your asthma is well-controlled. The highest number you get during that time is your personal best. You can compare this number to future numbers to make sure your asthma is controlled.
Your peak flow meter can help warn you of an asthma attack, even before you notice symptoms. If your score shows that your breathing is getting worse, you should take your quick-relief medicines the way your asthma action plan directs. Then you can use the peak flow meter to check how well the medicine worked.
Get Asthma Checkups
When you first begin treatment, you’ll see your doctor about every 2 to 6 weeks. Once your asthma is controlled, your doctor may want to see you from once a month to twice a year.
During these checkups, your doctor may ask whether you’ve had an asthma attack since the last visit or any changes in symptoms or peak flow measurements. He or she also may ask about your daily activities. This information will help your doctor assess your level of asthma control.
Your doctor also may ask whether you have any problems or concerns with taking your medicines or following your asthma action plan. Based on your answers to these questions, your doctor may change the dose of your medicine or give you a new medicine.
If your control is very good, you might be able to take less medicine. The goal is to use the least amount of medicine needed to control your asthma.
Emergency Care
Most people who have asthma, including many children, can safely manage their symptoms by following their asthma action plans. However, you might need medical attention at times.
Call your doctor for advice if:
- Your medicines don’t relieve an asthma attack.
- Your peak flow is less than half of your personal best peak flow number.
Call 9-1-1 for emergency care if: Note* This is only for people who live in USA.
- You have trouble walking and talking because you’re out of breath.
- You have blue lips or fingernails.
At the hospital, you’ll be closely watched and given oxygen and more medicines, as well as medicines at higher doses than you take at home. Such treatment can save your life.
Asthma Treatment for Special Groups
The treatments described above generally apply to all people who have asthma. However, some aspects of treatment differ for people in certain age groups and those who have special needs.
Children
It’s hard to diagnose asthma in children younger than 5 years. Thus, it’s hard to know whether young children who wheeze or have other asthma symptoms will benefit from long-term control medicines. (Quick-relief medicines tend to relieve wheezing in young children whether they have asthma or not.)
Doctors will treat infants and young children who have asthma symptoms with long-term control medicines if, after assessing a child, they feel that the symptoms are persistent and likely to continue after 6 years of age.
Inhaled corticosteroids are the preferred treatment for young children. Montelukast and cromolyn are other options. Treatment might be given for a trial period of 1 month to 6 weeks. Treatment usually is stopped if benefits aren’t seen during that time and the doctor and parents are confident the medicine was used properly.
Inhaled corticosteroids can possibly slow the growth of children of all ages. Slowed growth usually is apparent in the first several months of treatment, is generally small, and doesn’t get worse over time. Poorly controlled asthma also may reduce a child’s growth rate.
Many experts think the benefits of inhaled corticosteroids for children who need them to control their asthma far outweigh the risk of slowed growth.
Older Adults
Doctors may need to adjust asthma treatment for older adults who take certain other medicines, such as beta blockers, aspirin and other pain relievers, and anti-inflammatory medicines. These medicines can prevent asthma medicines from working well and may worsen asthma symptoms.
Be sure to tell your doctor about all of the medicines you take, including over-the-counter medicines.
Older adults may develop weak bones from using inhaled corticosteroids, especially at high doses. Talk with your doctor about taking calcium and vitamin D pills, as well as other ways to help keep your bones strong.
Pregnant Women
Pregnant women who have asthma need to control the disease to ensure a good supply of oxygen to their babies. Poor asthma control increases the risk of preeclampsia, a condition in which a pregnant woman develops high blood pressure and protein in the urine. Poor asthma control also increases the risk that a baby will be born early and have a low birth weight.
Studies show that it’s safer to take asthma medicines while pregnant than to risk having an asthma attack.
Talk with your doctor if you have asthma and are pregnant or planning a pregnancy. Your level of asthma control may get better or it may get worse while you’re pregnant. Your health care team will check your asthma control often and adjust your treatment as needed.
People Whose Asthma Symptoms Occur With Physical Activity
Physical activity is an important part of a healthy lifestyle. Adults need physical activity to maintain good health. Children need it for growth and development.
In some people, however, physical activity can trigger asthma symptoms. If this happens to you or your child, talk with your doctor about the best ways to control asthma so you can stay active.
The following medicines may help prevent asthma symptoms caused by physical activity:
- Short-acting beta2-agonists (quick-relief medicine) taken shortly before physical activity can last 2 to 3 hours and prevent exercise-related symptoms in most people who take them.
- Long-acting beta2-agonists can be protective for up to 12 hours. However, with daily use, they’ll no longer give up to 12 hours of protection. Also, frequent use of these medicines for physical activity might be a sign that asthma is poorly controlled.
- Leukotriene modifiers. These pills are taken several hours before physical activity. They can help relieve asthma symptoms brought on by physical activity.
- Long-term control medicines. Frequent or severe symptoms due to physical activity may suggest poorly controlled asthma and the need to either start or increase long-term control medicines that reduce inflammation. This will help prevent exercise-related symptoms.
Easing into physical activity with a warmup period may be helpful. You also may want to wear a mask or scarf over your mouth when exercising in cold weather.
If you use your asthma medicines as your doctor directs, you should be able to take part in any physical activity or sport you choose.
People Having Surgery
Asthma may add to the risk of having problems during and after surgery. For instance, having a tube put into your throat may cause an asthma attack.
Tell your surgeon about your asthma when you first talk with him or her. The surgeon can take steps to lower your risk, such as giving you asthma medicines before or during surgery.
You can’t prevent asthma. However, you can take steps to control the disease and prevent its symptoms. For example:
- Learn about your asthma and ways to control it.
- Follow your written asthma action plan.
- Use medicines as your doctor prescribes
- Identify and try to avoid things that make your asthma worse (asthma triggers). However, one trigger you should not avoid is physical activity. Physical activity is an important part of a healthy lifestyle. Talk with your doctor about medicines that can help you stay active.
- Keep track of your asthma symptoms and level of control.
- Get regular checkups for your asthma.
For more details about how to prevent asthma symptoms and attacks, go to “How Is Asthma Treated and Controlled?”
If you have asthma, you’ll need long-term care. Successful asthma treatment requires that you take an active role in your care and follow your asthma action plan.
Learn How To Manage Your Asthma
Partner with your doctor to develop an asthma action plan. This plan will help you know when and how to take your medicines. The plan also will help you identify your asthma triggers and manage your disease if asthma symptoms worsen.
Children aged 10 or older -and younger children who can handle it -should be involved in creating and following their asthma action plans.
Most people who have asthma can successfully manage their symptoms by following their asthma action plans and having regular checkups. However, knowing when to seek emergency medical care is important.
Learn how to use your medicines correctly. If you take inhaled medicines, you should practice using your inhaler at your doctor’s office. If you take long-term control medicines, take them daily as your doctor prescribes.
Record your asthma symptoms as a way to track how well your asthma is controlled. Also, your doctor may advise you to use a peak flow meter to measure and record how well your lungs are working.
Your doctor may ask you to keep records of your symptoms or peak flow results daily for a couple of weeks before an office visit. You’ll bring these records with you to the visit. (For more information about using a peak flow meter, go to “How Is Asthma Treated and Controlled?”)
These steps will help you keep track of how well you’re controlling your asthma over time. This will help you spot problems early and prevent or relieve asthma attacks. Recording your symptoms and peak flow results to share with your doctor also will help him or her decide whether to adjust your treatment.
Ongoing Care
Have regular asthma checkups with your doctor so he or she can assess your level of asthma control and adjust your treatment as needed. Remember, the main goal of asthma treatment is to achieve the best control of your asthma using the least amount of medicine. This may require frequent adjustments to your treatments.
If you find it hard to follow your asthma action plan or the plan isn’t working well, let your health care team know right away. They will work with you to adjust your plan to better suit your needs.
Get treatment for any other conditions that can interfere with your asthma management.
Watch for Signs That Your Asthma Is Getting Worse
Your asthma might be getting worse if:
- Your symptoms start to occur more often, are more severe, or bother you at night and cause you to lose sleep.
- You’re limiting your normal activities and missing school or work because of your asthma.
- Your peak flow number is low compared to your personal best or varies a lot from day to day.
- Your asthma medicines don’t seem to work well anymore.
- You have to use your quick-relief inhaler more often. If you’re using quick-relief medicine more than 2 days a week, your asthma isn’t well controlled.
- You have to go to the emergency room or doctor because of an asthma attack.
If you have any of these signs, see your doctor. He or she might need to change your medicines or take other steps to control your asthma.
Partner with your health care team and take an active role in your care. This can help you better control your asthma so it doesn’t interfere with your activities and disrupt your life.